Billing Services
3-4%
per month
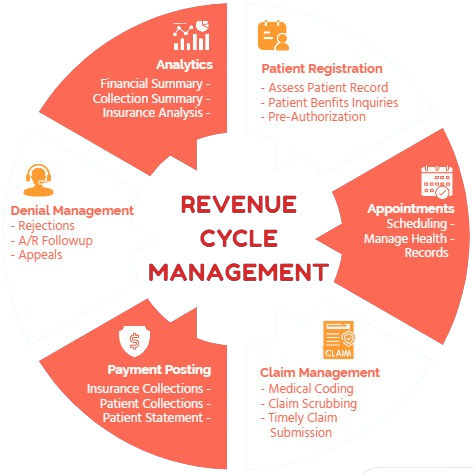
- Patient Insurance Verification
- Coding
- Claim Scrubbing
- In Time Claim Submission
- AR Follow up
Services We Provide
✓ Proper benefit inquiries and prior authorizations where necessary.
To ensure a smooth billing experience, our team verifies insurance benefits specific to
service and estimates patient out-of-pocket expense. We also proactively check prior
approvals to avoid claim denials.
✓ Finalized Coding/Billing within 24 Hours
We ensure timely claims creation and submission to insurances within 24 hours, which
enhances the pace of your revenue cycle and you get paid early.
✓ Coding Verification Prior to submission
Our thorough claims scrubbing review process ensures accuracy by verifying codes
against the latest CMS guidelines (CCI edits, LCDs & NDCs) for a smooth billing
experience in first attempt.
✓ Timely follow up on Rejected Claims on submission
Our vigilant billing team closely monitors submitted claims and swiftly addresses any
rejections within 24 hours, ensuring faster claim approval by insurance.
✓ No aging beyond 15 days
Our claim follow up process starts from 15 days of claim submission. Which gives us
benefit of handling any denial in timely manner.
✓ 30/60/90 Days Follow Up cycle
Our Claims follow up cycle continues on the basis of 30/60/90 days of claims
submission. Keeping a steady track of our corrective actions taken against denials is our
top priority until claim is fully paid. Our observant account receivables team ensures
that no unpaid claim left unattended and maximizing the claims reimbursement by
implementing different follow up protocols.
✓ Patient billing services
We provide patient billing options. Upon applying any amount towards patient
responsibility, our billing team will send patient statements following provider SOP and
promptly notify the front desk to collect patient balances from patients.
✓ Credentialing for new and existing clients
Our credentialing and enrollment services help clients become in-network providers
with all major government and commercial insurances in any state. Our credentialing
expertise ensures you're in-network with major insurers. This allows you to see more
patients and grow your revenue.
✓ Accuracy
Transcribes medical dictations with precision, ensuring all details are captured without errors.
✓ Medical Terminology
Possesses a strong understanding of medical terminology, abbreviations, and jargon to transcribe effectively.
✓ Confidentiality
Maintains strict confidentiality of patient information, adhering to HIPAA regulations and ethical standards.
✓ Attention to Detail
Pays close attention to detail, including nuances in language and context, to produce accurate transcriptions.
✓ Efficiency
Works efficiently to meet tight deadlines while maintaining quality standards.
✓ Technology Proficiency
Utilizes transcription software and tools effectively to enhance productivity and accuracy.
✓ Continual Learning
Stays updated with medical advancements, terminology changes, and transcription best practices through ongoing education and training.
✓ Appointment Scheduling & Management:
Reduce phone tag and free up your front desk with efficient appointment scheduling and confirmations.
✓ Prior Authorization Processing:
Ensure timely approvals by handling prior authorization requests with accuracy and follow-through.
✓ Patient Communication & Support:
Enhance patient experience with professional communication and address inquiries efficiently.
✓ Referral Management
Streamline the referral process by coordinating with specialists and expediting appointments.
.
per month
per month
per month